Home > Publications > Policy Briefs > 5/ Looking at mothers differently to understand the feeding of children (...)
– The today Ivoirian mothers practices regarding the feeding of their children have an alarming impact on the children’s health.
– This is not due to the misreading of the good practices but to the di iculty they have to find balance between the multiple constraints they come across as wives, mothers and working women.
– This social approach must be taken into account to build more e icient nutritional interventions and public health policies.
Anaemia and malnutrition represent a very significant public health problem in Ivory Coast. In 2008, iron deficiency anaemia affected 81% of children of under 5 years of age and 59% of women of a reproductive age in the north of the country, as well as 75% of children of under 5 years of age and 68% of reproductive age in Abidjan (PNN, 2010). Moreover, according to the MICS 2012, 75% of children aged 6-59 months are anaemic: 25% in a light form, 46% in a moderate form and 3% in a severe form.
Additionally, the high prevalence of malnu-trition and the precariousness of the state of nutrition, in particular for children aged less than 5 years also brought about retarded growth for 30% of children in 2011 (MICS 2012).
According to the Programme National de Nutrition en Côte d’Ivoire (PNN—Ivory Coast national nutrition programme) and the World Health Organisation (WHO), bad feeding practices, due in particular to a lack of knowledge of the correct practices to follow, are consid-ered as the key causes of the nutritional situation of the mother-child pair (PNN 2010 and WHO 2003). However, various works in other countries show that feeding practices are not solely determined by knowledge of nutrition (Calandre, 2009). In Ivory Coast, determining factors of feeding practices have been studied little recently, with the most recent works dating back to more than 20 years ago (Akindès, 1991). Moreover, few sociological studies have been carried out on the practices of child feeding and their determining factors, whether in Ivory Coast or in other countries in Africa (PNN 2010).
It is in order to understand the determining factors of feeding practices that this study was carried out, focusing on the following two questions:
➜ Are the feeding practices of mothers very different from the nutritional recommendations of the WHO?
➜ What are the constraints and factors for women which underlie these practices?
In order to provide an answer, a team of socio-anthropologists carried out a qualitative study on the practices of infant feeding adopted by mothers and grandmothers, as well as the factors which explain them.
Comparison between the recommendations of international norms and those of older women relating to child nutrition, along with the practices of mothers, revealed some significant discrepancies.
Standardised nutritional norms
Since 2001, the WHO and Unicef have recom-mended that mothers should exclusively give moth-er’s milk to their baby for the first 6 months of their life, since this contains all of the nutrients which are essential for its development. Neither drinking water nor complementary foods are recommended before the age of 6 months. The latter can be introduced from the age of six months onwards (180 days), while continuing to breastfeed. The period of dietary diversification then begins, in which it is recommended to progressively introduce gruels of cereals, vegetables, fruits, fishes and then meats (WHO 2003).
The norms conveyed by the older women
For the older women, the child should be fed with mother’s milk for the first 8 months of its life, as was done previously according to them. In their view, water should be offered from birth onwards (in addi-tion to mother’s milk) because “the child is a human who is thirsty as well, like adults” and complemen-tary foods should only be introduced from 8 months onwards.
Itineraries and practices which are particular to mothers
The mothers in our sample uniformly identify four major phases in the feeding of the child:
➜ a phase of breastfeeding which they call “exclusive” from 0 to 3 months but which, for some, has a tendency to be shortened, with the introduction of water from birth;
➜ a second phase, of weaning or dietary diversification, which begins between 3 and 5 months with the introduction of liquid gruels which are then thickened;
➜ a third phase, from 5 to 7 months, of continuation of the diversification in which the child gains the experience not only of thick gruels, but also of soft solids, its first savoury foods;
➜ from 8 months onwards, where the child gains experience with solid foods and progressively discovers the dishes reserved for other members of the household.
With dietary diversification, from 3 months onwards, it is the frequency of breastfeeding which drops, as the mother is generally no longer available to fulfil the breastfeeding needs of the child (multiple reasons linked with the demands of the urban envi-ronment). Complete stopping of breastfeeding gener-ally occurs at around 15 – 16 months.
For each of these phases, even if we observe variations in the mode of preparation and presentation from one mother to another, in all the cases their practices correspond neither to nutritional recommendations nor to the norms conveyed by the elder women (the grandmothers). There is in fact a discrepancy in the favoured duration of so-called “exclusive” breastfeeding and the age at which foods are introduced. Moreover, it is observed that the period of weaning and diversification from 3 months onwards, which is mentioned by the women, is not recognised. Finally, the breastfeeding described as “exclusive” by the WHO is not recognised, either by the older women or by the mothers, since water is introduced from birth onwards.
What explains this discrepancy? Even if they know the recommendation to breastfeed exclusively up to the age of 6 months, women explain their difficulty in waiting for this time to introduce foods supplementing the mother’s milk. In fact, even though they clearly seek the well-being of their chil-dren, mothers today are subject to demands which are not the same as those of their elders were.
Strong economic constraints and time constraints - as an economically active woman
Today, in an urban environment, both parents participate in bearing the financial burden of the household, which was not the case for their elders. Many women have to resume their professional and commercial activities, in particular if they were working independently. They therefore need to manage their time, and are obliged to leave their child as soon as possible (sometimes from six weeks onwards). It is therefore difficult for them to devote themselves entirely to their child, to breastfeed it as often as it would like during the day, and even more to wait until the child has reached the age of six months or even eight months (according to the older women) before introducing the first foods as a complement to breastmilk. Hence this introduction allows them to delegate the nursing function to a third party person in order to be able to go and work.
In day-to-day life, women also use “time-saving tactics”. They introduce complementary foods early when feeding their child in order to get it to sleep quickly and for a longer time.
Issues linked with the aesthetics of the body and life in a couple – as a wife
Previously the older women, who were often the wives of polygamous husbands, lived separately from their husbands from pregnancy onwards, until the child reached the age of two and a half (until they no longer breastfed). They therefore had the time to devote themselves to breastfeeding their child during the time which they spent away from their husband, which is no longer the case of mothers who emerge from itineraries of female emancipation and a choice of life overdetermined by the idea of a couple in a nuclear family, in a social environment which was rather unfavourable to the realisation of such an ideal: “the husbands are already fickle, imposing 30 months of absti-nence postpartum to your husband is equivalent to throwing him into the arms of other women, with all the risks that brings: sexually transmissible diseases, definitive separation, etc.” (interview with Adjoua, Abidjan). The reduction of the phase of exclusive breastfeeding and the advancement of the diversi-fication and weaning of the child may therefore be read partially as the search for a more harmonious relationship with the husband, and the confir-mation, in this sense, of the role of wife and the identity of a woman. Hence the stopping of breast-feeding definitively marks the end of the period of permanent attention surrounding the feeding of the child. It also marks the end of a double pressure on the mother: the pressure created by the fear of touching the child after sexual relations with the husband, and the pressure linked with aesthetics: breasts which are no longer subject to the risk of becoming “saggy when the child breastfeeds too much” (Alphonsine Y., Abidjan).
Nutritional issues and those relating to socialisation – as a mother
The woman, as a mother, must guarantee and satisfy the nutritional needs of her child. She must pay great attention to the culinary preparation of meals and the choice of ingredients.
She must also take care of issues relating to the socialisation and identity of her child by preparing homemade gruels based on local cereals, by integrating the child in the family meal, and by educating it in the taste and texture of dishes which are seen as relevant for their identity.
Between nutritional recommendations, the statements of older women (grandmothers), changes in the image of the woman (today no longer solely a “nurturer” but also an economically active woman and a wife), women find themselves in the middle of a plurality of social norms and a plurality of infor-mation (media, professionals, and older people). They therefore have to make decisions and permanent choices which are also influenced by constraints (economic, temporal, or other) with which they are confronted. This makeshift product is transformed into a social law, or even a ‘norm of feeding practice’. The feeding practices which structure these norms are those which mothers adopt for their children, and which are therefore only a combination of all of these influences. There is no single, simple reason which can allow them to be explained. Moreover, it may be thought that this context also generates anxiety, and it should be considered that mothers ultimately do “everything they can” to assure the well-being of their children considering all of the burdens which they bear and the pressures which they manage.
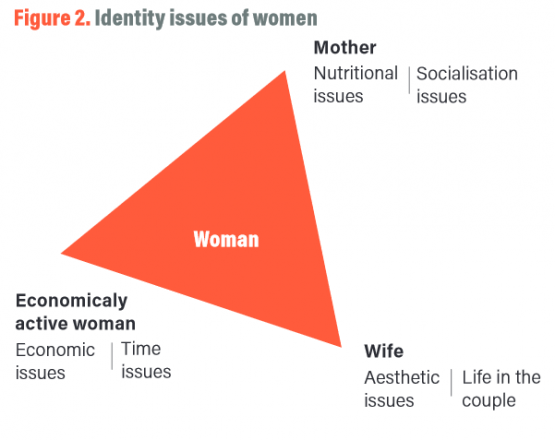
The study displayed discrepancies between nutritional norms and mothers’ practices in feeding children, which with time are instituted as ‘standard practices’. Putting the issue in terms of a discrepancy gives rise to the idea of ignorance or imperfection. This kind of representation often leads to suggestions to provide better education or training for mothers, with better knowledge inducing better practices. However, the study shows that if mothers do not apply rules which they know only too well, it is because beyond their function as mothers, they are also subject today to constraints linked with their status as an economically active woman and wife.
This kind of result suggests no longer reducing women uniquely to their role as nursing mothers. Instead it provides a stimulus to take into account the plurality of their identities and their difficulties in making decisions between their professional and social constraints and the management of their body and their couple.
– Francis AKINDES, Gisèle SEDIA, Gisèle KOUAKOU, UNESCO Chair in Bioethics, Bouaké, Ivory Coast
– Anne BERCHON, Nicolas BRICAS, Cirad, Montpellier, France
KINDES Francis, 1991, Restauration populaire et sécurité alimentaire à Abidjan, in Cahier des Sciences Humaines, n° 27, pp 169-179.
CALANDRE Natacha, BRICAS Nicolas, SIRIEIX Lucie, 2009, Comment les mères perçoivent-elles les risques nutritionnels de leurs enfants ? Une approche par le paradigme psychométrique au Vietnam, in Economies et sociétés, pp 1735-1760.
INS (Institut National de la Statistique) et ICF International, 2012, Enquête Démographique et de Santé et à Indicateurs Multiples de Côte d’Ivoire 2011-2012, Calverton, Maryland, USA : INS et ICF International, 591 p.
OMS, 2003, Stratégie mondiale pour l’alimentation du nourrisson et du jeune enfant, 36 p.
PNN (Programme National de Nutrition), 2010, Rapport du Landscape Analysis pour la Côte d’ivoire, 74 p.
